Background: Dominantly inherited β-Thalassemia (β-thal) is a rare condition that results from a heterozygous mutation in the β-globin gene ( HBB), leading to the synthesis of an unstable β-globin chain, most frequently an elongated protein. Although heterogeneous, it presents not as β-thalassemia trait but rather with a more severe phenotype, resembling β-thal major or intermedia, with chronic hemolytic anemia and splenomegaly. There are approximately 150 known dominantly inherited α- and β-globin gene mutations (http://globin.cse.psu.edu/). We present a case of a novel HBB mutation leading to a dominant form of β-thalassemia, outlining our approach to attaining an appropriate diagnosis and management leading to transfusion independence.
Case: A 32-year-old Caucasian female was referred to our center with a diagnosis of congenital dyserythropoietic anemia type II (CDA-II), based on bone marrow studies at 12 years of age which had demonstrated a hypercellular marrow with erythroid hyperplasia and 10% binucleated red cells. Molecular testing had not been performed. Her history was negative for developmental delay, growth retardation, or family history of anemia. She had presented to medical attention at age 11 with symptomatic anemia. Prior treatments included steroids, IVIG, and erythropoietin, with no significant improvement of her anemia. She underwent splenectomy at 19 years of age due to the hemolytic component of her anemia with the clinical diagnosis of CDA-II, with a mild improvement in baseline hemoglobin from 70-80g/L to 80-90g/L. Spleen pathology demonstrated splenomegaly (weight of 1kg) and mild iron deposition.
At the time of presentation at our centre, her predominant symptom was fatigue, for which she was initiated on a chronic transfusion protocol, to maintain a pretransfusion hemoglobin of 90 g/L; she received a total of 53 units from October 2018 to November 2022. She subsequently developed worsening iron overload (ferritin 888, TSAT 80%, and LIC of 8.1mg of iron per gram of liver dry weight) requiring initiation of iron chelation therapy.
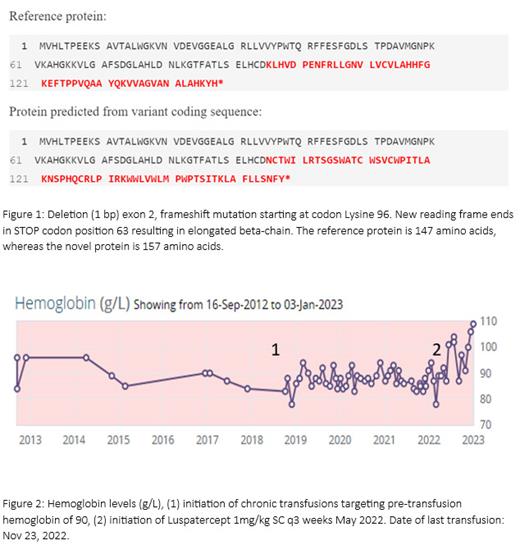
Given her presumptive diagnosis of CDA-II she was later enrolled in the Congenital Dyserythropoietic Anemia Registry (CDAR) for North America (https://www.clinicaltrials.gov/study/NCT02964494). Molecular testing by next generation sequencing (NGS) on a CDA gene-panel at that time failed to identify a causative CDA mutation. Further testing with whole exome sequencing revealed a one base-pair deletion in exon 2 of the β-globin gene, creating a frameshift variant at codon 96 and ending in a premature STOP, 63 codons downstream p.(Lys 96Asnfs*63) (Figure 1). This mutation led to an elongated β-globin chain and an unstable hemoglobinopathy predicted to be the cause of her presentation. Hemoglobinopathy screen revealed HBF 8.7%, HBA 87.5%, and HBA2 3.8%.
Based on the above testing, a diagnosis of dominant β-thalassemia intermedia due to HBB NM_00518.4, c.288delG, p.K96fs, recognizing that she had been previously misdiagnosed with CDA-II. Based on the revised diagnosis, the patient was initiated on Luspatercept 1mg/kg SC q3 weeks, with rapid improvement in her pre-transfusion hemoglobin to >100g/L as well as in her symptomatology and quality of life (Figure 2), rendering her transfusion independent.
Discussion: This case report, to our knowledge, demonstrates a novel β-globin gene mutation leading to dominant β-thalassemia, with the phenotype of β-thal-intermedia. The latency between presentation and diagnosis demonstrates the challenges associated with diagnosing rare hemolytic anemias and highlights the importance of molecular testing to confirm the diagnosis, especially before proceeding to splenectomy which may predispose to vasculopathies in some of these diseases, such as congenital dyserythropoietic anemia type I and unstable hemoglobinopathies.
Disclosures
Uminski:Takeda: Honoraria; BioCryst Pharmaceuticals: Honoraria; Bayer: Research Funding; Novo Nordisk: Other: Educational Grant; Roche: Other: Educational Grant; CSL Behring: Other: Educational Grant. Kalfa:Agios Pharmaceuticals, Inc.: Consultancy, Research Funding; Forma/Novo Nordisk: Consultancy, Research Funding. Goodyear:Medison: Honoraria; Roche: Honoraria; Alexion: Honoraria; Sanofi: Honoraria; Sobi: Honoraria; Pfizer: Honoraria; CSL Behring: Honoraria; BioCryst Pharmaceuticals: Honoraria; Takeda: Honoraria. Rydz:Pfizer: Honoraria; Chiesi: Honoraria; Sobi: Honoraria; Vertex Pharmaceuticals: Honoraria; Bayer: Honoraria; BMS: Honoraria; Novo Nordisk: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal